Quality measures are one of 3 domains used by CMS to determine your nursing home’s 5-Star Rating:
- Health Inspection
- Staffing
- Quality Measures
Quality measures target specific indicators of the level of care provided at your nursing home.
They include data on resident and staff vaccinations, pressure ulcer treatment and prevention, and the frequency of residents' falls.
While CMS monitors staffing under a separate domain, it directly impacts your quality measures ratings. Because without adequate, highly skilled staff working each shift, the quality of care just won’t be up to par.
So whether you want to improve ✶quality measures rating✶ or elevate the overall resident experience, upgrading staff scheduling is the best place to start.
Try these 7 strategies to improve your quality measures rating to offer better resident care (and upgrade your employee experience).
- 1. Rehospitalization and ER Visits
- 2. Pressure Ulcers: Prevalence & Prevention
- 3. Falls & Major Injuries
- 4. Medication Management: Antipsychotic Meds
- 5. Immunizations: Prevention is the Best Treatment
- 6. Mobility & Functional Status
- 7. Behavioral Health: Depressive & Behavioral Symptoms
- MakeShift’s Smarter Scheduling Can Help Improve Quality Measures
1. Rehospitalization and ER Visits
Reducing rehospitalization and ER visits is crucial for improving the quality of care in nursing homes and your rating.
By understanding the factors that contribute to these issues, such as poor care transitions, insufficient communication, and inadequate staff training and staffing, you can implement effective strategies to improve this area.
If nursing homes send many residents back to the hospital or the ER, it may be because they aren't adequately assessing or caring for them.
If your hospital readmission rate is high, it’s urgent that you get to the root of the problem.
A 2022 report cited less than 53% of short-stay patients have successful discharges (meaning no hospital re-admission).

Here’s how to reduce ER trips and return hospital visits:
Implement robust care transition protocols — Ideas for comprehensive protocols:
- Coordinating care directives from the hospital, including complications to watch for.
- Including residents and their families in the care plan discussion.
- Extra resident “check-ins” for 48 to 72 hours after hospital discharge.
- Use telemedicine services to consult with hospital specialists for timely interventions to prevent an ER trip.
Enhance staff training on recognizing (and how to intervene) early signs of health deterioration — Signs can include:
- Sleep disturbances
- Depression
- Pain
- Change in appetite
- Fatigue
- Breathing changes
Utilize scheduling software to ensure adequate staff coverage — An AI-powered scheduling solution can automatically help ensure safe nurse-to-patient ratios.
Optimal scheduling helps prevent burnout, which can hinder empathy and care quality — both directly impact hospital readmission rates.
2. Pressure Ulcers: Prevalence & Prevention
This measure focuses on the percentage of residents with pressure ulcers.
Pressure ulcers, also known as pressure injuries, bed sores, and deep tissue injuries, are areas of damaged skin caused by long-term pressure, like staying in one position for too long.
Pressure ulcers/injuries can be excruciating and cause other complications, such as reduced mobility and infections.
Approximately 8.5% of nursing home residents acquire some sort of pressure ulcer.
Here’s how to reduce pressure ulcers:
Perform regular skin assessments & pressure ulcer risk evaluations. Critical aspects of evaluation include:
- Mobility — The patient's ability to move independently because limited mobility increases the risk of pressure ulcers.
- Nutritional status — The patient's nutritional intake — poor nutrition can impair skin integrity and healing.
- Moisture exposure — Monitor for excess moisture from sweating, incontinence, or wound drainage, which weakens the skin.
- Sensory perception — The ability to feel and respond to pressure-related discomfort.
- Existing health conditions — Chronic illnesses or conditions may affect skin health or circulation, for example, diabetes or vascular disease.
Increase staff awareness and training on proper skin care and repositioning techniques.
Schedule adequate staff to ensure a proper nurse-to-patient ratio to provide consistent care and timely repositioning.
3. Falls & Major Injuries
This measures the number of residents who experienced falls with significant injuries. A high number could indicate a facility’s low quality of care or lack of patient awareness.
Approximately half of nursing home residents fall every year. About 1 in 3 of those who fall will fall 2 or more times in a year. Falls often have serious consequences, especially in frail older residents.

Increase your fall prevention efforts by:
- Conducting regular fall risk assessments
- Implementing physical therapy & balance training programs
- Equipping your facility with safety features like handrails & non-slip flooring.
4. Medication Management: Antipsychotic Meds
This measures the percentage of your residents receiving antipsychotic medications. Antipsychotic drugs are an important treatment for patients with certain mental health conditions.
However, the FDA has warned that when antipsychotic medications are used in elderly patients with dementia, they’re 1.7 times more likely to die.
Managing behavior without using medications, like higher staffing ratios and varied activities (gardening, art, massage), has lowered the need for medications in many cases.
Here are some tips to lean less on antipsychotic meds:
- Take a holistic approach — Consider medical, psychological, social, and environmental factors impacting a resident. Offer activities that promote social engagement. Assess for pain, infections, or other medical conditions that could cause behavioral changes.
- Consider behavioral therapy — Use behavioral therapies to address and modify challenging behaviors. Train staff in techniques like cognitive-behavioral therapy (CBT) and other behavior management strategies.
- Schedule staff to offer personalized care and activities — This requires careful shift planning based on roles and skills to ensure patients have access to activities and therapy that’ll help them reduce medication. (Massage therapists, activity leaders, behavioral therapists, etc.)
5. Immunizations: Prevention is the Best Treatment
This measure tracks the percentage of healthcare workers and residents who’ve received the flu vaccine each flu season. It applies to ALL facility employees, licensed independent practitioners, adult students/trainees, and adult volunteers.
The flu can be more dangerous for older adults because their immune systems weaken with age, making them more susceptible to secondary infections like pneumonia.

Unfortunately, the leading cause of death among nursing home residents is pneumonia.
You can reduce the risks by focusing on prevention:
- Educate residents & families about the importance of vaccinations
- Coordinate with healthcare providers to make getting vaccinated easily accessible.
6. Mobility & Functional Status
This focuses on the percentage of residents whose ability to move around and care for themselves improved. Examples of mobility improvements are:
- Transferring (for example, from the bed to a chair)
- Getting around the nursing home unit
- Walking in the hallway
How well a person gets around and can care for themselves directly impacts their ability to thrive, which is why CMS measures these areas.
Improvement in Mobility
Almost 90% of long-term care residents have limited mobility, associated with a loss of ability in daily living activities. Limited mobility increases the risk of falls, pressure ulcers, incontinence, and a significant decline in health-related quality of life.
You can help improve mobility through:
- Daily activity — Incorporate mobility exercises into daily routines. For example, encourage walking to meals or activities. Encourage patients to participate in group exercises and mobility-enhancing activities, including daily activities they’ll do at home.
- Tailored physical therapy programs — Create individualized exercise and rehabilitation plans to improve strength and balance.
Self-Care Improvement
The ability to care for oneself is a significant factor in quality of life — this applies to both long-term and short-term residents.
- Help residents improve how well they care for themselves through:Personalized care plans focusing on self-care skills
- Implement adaptive equipment and environmental modifications
- Offer workshops on daily living skills, like using new medical equipment or managing finances. Based on your residents’ needs, expand to individual occupational therapy sessions.
- Use scheduling software to incorporate occupational therapists for self-care training into your staff schedule.
7. Behavioral Health: Depressive & Behavioral Symptoms
This measures the percentage of residents with depressive or behavioral symptoms that affect others.
3 examples of behavioral symptoms are:
- Aggression or irritability — Depression and other behavioral symptoms can sometimes manifest as aggression or irritability, which can create tension and fear among other residents.
- Crying & distress — Frequent crying or expressions of distress can be unsettling for other residents and potentially affect their emotional well-being.
- Negative talk & hopelessness — Constant negative talk or expressions of hopelessness can affect the morale of other residents, possibly leading to a more pessimistic atmosphere within your nursing home.
A high percentage of nursing home residents have a significant mental disorder, ranging from 65% to 91%, so awareness of behavioral issues is essential.
Here’s how to support your residents’ mental health:
- Conduct regular mental health screenings.
- Regularly check in with your residents — ask them how they’re doing.
- Offer counseling, social activities, and support groups.
- Schedule mental health professional visits and activities to boost morale.
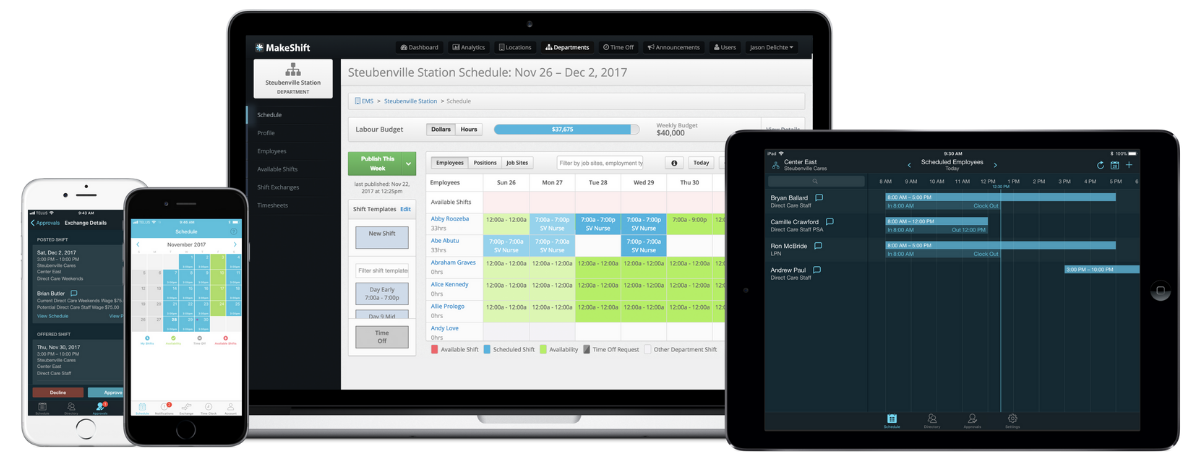
How Smarter Scheduling Can Help Improve Quality Measures
The proper scheduling of your nursing home staff is interwoven with the ranking of your quality measures. If you have measures you’d like to improve, focus on better staff allocation first. Often, poor quality of care directly correlates with understaffing.
MakeShift simplifies and streamlines scheduling while also offering suggestions for better shift coverage. Through true automation, you can spend 55% less time creating schedules.
We support nursing home staff scheduling in 4 powerful ways:
1. Shift planning is simple with our AI-powered scheduling platform (schedule nursing staff, therapists, and activities leaders automatically).

2. Easily schedule based on roles & skills to ensure you’ve got the right people scheduled for each shift. Add employee skills to their profile, then ask ShiftMate AI to offer schedule suggestions based on expertise and availability.

3. MakeShift allows interactive scheduling where staff can input availability, time off, or shift swap requests and access their schedules from their phones.
When your staff has more say in their schedules, you’ll see an increase in engagement, morale, and retention. These factors affect your employees’ capacity to provide a high level of care.

4. Simplified communication through a single channel. Rather than using texting, multiple social media platforms, DM’s, and email — all communication flows through the MakeShift messaging app. No missed messages or misunderstandings due to communication delays or gaps.

Upgrade Your Staff Scheduling ↠ Improve Your Quality Measures Rating
Adequate staffing directly and indirectly impacts your facility’s quality of care, which correlates with your CMS five-star rating.
Want to improve your nursing home’s quality measures ratings? Focus on stellar staff scheduling. When you have the right number of people with the right skills on each shift, the quality of care increases.
Don’t go it alone. MakeShift offers exceptional support and smart scheduling to get your facility up and running fast. Want to take it for a test drive? Try it for FREE with our 14-day trial.