Baby boomers are retiring left and right, which means some of them will need long-term care in the future.
The heavy load on nursing homes is growing:
- Someone who turns 65 today has almost a 70% chance of needing some type of long-term care services and support.
- Women need care longer (3.7 years) than men (2.2 years)
- 1/3 of today's 65-year-olds won’t need long-term care support. But of those that do, 20% will need it longer than 5 years.
The demand is also growing in your industry.
You’ll need more beds and more staff. Not to mention, Boomers are known for loving the good life, so you’ll need higher-level amenities if you want to keep them happy.
With all this upcoming demand, how do you know what to prioritize?
Relax.
We created a comprehensive list of the latest nursing home stats and trends, plus ideas on how to implement them.
By the end of this report, you’ll know how to upgrade your facility and patient care while prioritizing your staff’s well-being.
- Nursing Home Statistics You Can’t Afford to Miss
- Why Do Long-Term Care Statistics Matter?
- Need-To-Know Nursing Home Statistics & Trends
- FAQ
- How MakeShift Elevates Nursing Home Staff Scheduling
- Let the Stats and Trends Guide You
Nursing Home Statistics You Can’t Afford to Miss
While this article is packed with the latest stats and trends to upgrade your facility and employee experience, we’ve cherry-picked our top 5 to highlight here.
1. Approximately 10,000 baby boomers will reach retirement age EVERY DAY from 2011 through 2030.
2. The majority of residents in nursing homes are women, ranging between 62.8% & 63.3% of the resident population.
3. Roughly ½ of all nursing home residents suffer a fall at least once a year. Many have complications after the fall.
4. A study of 470 nursing home residents with access to an outdoor garden experienced:
- 36% improvement in general health
- 35% higher life satisfaction
- 21% decrease in depression symptoms
Why Do Long-Term Care Statistics Matter?
Nursing home trends and statistics help you ready your facility for the future of long-term care.
The growing older population is driving the need for attention to these trends. As the number of older adults increases, so does the demand for nursing home services.
The global population of 60+ has more than doubled since 1980 and is projected to reach 2.1 billion by 2050.
This demographic shift shines a light on the need for strategic planning and resource allocation to handle the needs of a growing older population. By staying informed about trends and statistics, you can make data-driven decisions to:
- Enhance capacity
- Improve care quality
- Implement innovative solutions to meet residents’ diverse needs
- Elevate your staff’s work environment
With today’s focus on the quality of life for long-term care residents, you play a pivotal role in using trends and statistics as a guide.
Use this information to help you develop compassionate, people-centric care strategies that adapt to the changing needs of the elderly population.
Need-To-Know Nursing Home Statistics & Trends
You’ve heard the stats on the “Silver Tsunami.” Roughly 10,000 baby boomers will REACH RETIREMENT AGE EVERY DAY from 2011 through 2030. The 65+ age group has grown 58% over the past 30 years.
By 2050, more than 1 in 5 Americans will be 65 or older.
By 2030, the number of people aged 60+ will surpass the number of young people aged 15 to 24 for the first time in history.

With the rising aging population, let’s get into nursing home statistics and trends you can use to prep your facility.
Nursing Home Demographics
The demographics of nursing homes in the U.S. and Canada give insight into the diversity of long-term care in these countries.
By exploring demographics, you gain valuable insight into the evolving demands on nursing homes and the future of care quality and accessibility.
U.S. Demographics
- The majority of residents in nursing homes are women, 63.3% of the population, while men make up 36.7%

- Number of nursing homes: 15,300
- Number of beds: 1.6 million
- Of the more than 55.8 million elderly adults in the U.S. (65+), 1.3 million live in nursing homes, which is 2.3% of the elderly population.
- The number of elderly adults will grow from today’s 55.8 to 95 million by 2060.
Today’s nursing home residents:
- 16.9% are under the age of 65
- 19.5% are between 65 & 74
- 27.2% are between 75 & 84
- 36.4% are 85 or older
Canadian Demographics
- The majority of residents in nursing homes are women, 62.8%, while men make up 37.2%
- Number of nursing homes: 2,076
- Number of beds: 198,220
- There are 6.8 million people aged 65+ in Canada today. In 2020, the number of nursing and residential care facility residents fell 4.3% to 474,000.
Today’s nursing home residents:
✶ What you can do with this information:
- Diversify Services — Given the high percentage of women in nursing homes, try offering services and activities that meet their specific needs and preferences. Experiment with a variety of programs catering to women’s interests and health concerns:
- Fitness classes
- Social events
- Wellness programs - Plan for Aging Population — With the expected increase in the elderly population, you should plan for future expansion or renovation projects to accommodate more residents. This may include:
- Increasing the number of beds
- Enhancing facilities
- Investing in tech that improves care quality and efficiency - Address Younger Residents' Needs — Considering that a significant portion of nursing home residents are under 65, you must provide services and activities that cater to them. You could offer:
- Vocational rehab programs
- Adaptive sports
- Social activities that encourage interaction among younger residents
Nursing Home Resident Common Medical Conditions
Long-term care facilities cater to a population with complex health needs. Chronic illnesses, cognitive impairments, and physical disabilities are prevalent among residents, each presenting unique challenges for care and management.
Using these medical condition stats will help you develop targeted care plans and safe nurse-to-patient ratios, hire staff, allocate resources effectively, and ultimately enhance the quality of life for nursing home residents.
Residents in nursing homes typically have at least one chronic condition for which they need ongoing medical care.
All stats from US News:
- 27.6% of residents have arthritis
- 20.1% have some type of heart disease
- 34% have diabetes
- 76.9% have hypertension
- 48.8% suffer from depression
- 49.1% have Alzheimer’s disease or another form of dementia
- Approximately half fall every year. About 1 in 3 of those who fall will fall 2 or more times in a year. Falls often have serious consequences, especially in frail older residents.
- The leading cause of death among nursing home residents is pneumonia.
✶ What you can do:
- Implement Specialized Care Programs: With high rates of chronic conditions like diabetes, heart disease, and arthritis, consider implementing specialized care programs tailored to these illnesses. This could include:
- Hiring specialized healthcare professionals
- Providing ongoing staff training
- Ensuring access to necessary medical equipment & medications - Enhance Mental Health Support: Given the high prevalence of depression and dementia among residents, prioritize mental health support. This can involve:
- Hiring mental health professionals
- Offering onsite therapy and counseling services
- Creating programs that promote cognitive engagement & social interaction. - Focus on Fall Prevention: With approximately half of the residents experiencing falls annually, invest in fall prevention strategies. This can include:
- Conducting regular fall risk assessments
-Implementing physical therapy & balance training programs
-Equip your facility with safety features like handrails & non-slip flooring.
Statistics on Nursing Home Costs
The cost of a nursing home depends on many uncontrollable factors, such as the state, location, and residents' needs.
Different facilities offer a wide variety of options and features, private or shared rooms, and these differences drastically impact the cost of the nursing home.
They can range from budget-conscious to high-end.
In the U.S.:
- Medicare only pays for the 1st 100 days in a nursing home or skilled nursing facility, but only if specific criteria are met. Residents still have a copay during this time. When they reach day 101, Medicare coverage ends, and other forms of payment need to be in place.
- The average monthly cost of skilled nursing in a private room at a nursing home is $108,405 yearly, compared to just over $94,000 for a semi-private room.
- Alaska, Connecticut, & Hawaii have the highest daily costs for private nursing homes at $1,036, $499, and $464 daily. In Alaska, that adds up to a whopping $378,140 per year.
- Oklahoma, Louisiana, & Missouri are the least expensive areas, with per-day private room costs of $200, $199, and $195. In those states, the annual total is between $71,175 and $73,000.
In Canada:
- The residents & provincial government share nursing home costs. The Department of Health & Wellness pays for health care, and the resident pays for accommodation and personal expenses.
- Accommodation costs for facility care vary widely depending on location. Still, out-of-pocket expenses for long-term care in a facility could range from around $1,000 per month for ward-level accommodation in a government-subsidized facility to over $6,000 monthly for a private room in a non-subsidized facility.
- Vancouver and Toronto have the highest rates for private rooms at $4,628 to $4,481 per month (roughly $150/day).
- Kelowna area and Ontario have the least expensive options, ranging from $2,700 to $3,948 per month (roughly $90 - $130/day)
✶ What you can do to help resident families:
- Offer Flexible Pricing Options: Consider offering a range of pricing options to accommodate different budgets. This could include providing tiered pricing based on the level of care needed and creating packages that bundle services and amenities at a discounted rate.
- Provide Transparent Cost Breakdowns: Provide precise and detailed cost breakdowns to help residents and their families understand what they are paying for. Transparency can build trust and help families make informed decisions. This can include:
- Itemized charges for room & board
- Medical care
- Activities
- Extra services - Explore Alternative Funding Options: Educate residents and their families about alternative funding options such as:
- Long-term care insurance
- Veterans' benefits
- Medicaid (for those who qualify)
- Reverse mortgages
Offering financial planning services or partnering with financial advisors can help families navigate the complexities of funding long-term care.
7 Nursing Home Trends to Implement in Your Facility
Many nursing homes now take a more holistic approach to caring for their residents. They want to treat residents as complex individuals instead of treating only the symptoms that result from medical conditions.
They focus on cultivating wellness and improvement versus illness and maintenance. This idea has created a much-needed culture shift in many nursing homes.
Here are 7 of the latest trends and ideas to try them on a small scale in your facility.

1. Onsite Salon & Spa — Encourages self-care, offers convenience and independence (to make decisions for themselves), and social interaction.
- Aromatherapy and massage have been shown to benefit people with dementia. After a 5 -10 minute hand massage, dementia patients improved cognition and mood.
✶ What you can do:
- Start with offering basic salon services once a week, such as haircuts and manicures. Gradually introduce aromatherapy sessions and short hand massages as part of a relaxation program.

2. Fine Dining —This allows residents to feel like they’re actively participating in life instead of just eating to stay alive. A waiter serves residents, and they can order from a daily menu and even snag a table for their friends and family. The better-quality food served on porcelain plates feels more like a restaurant than a sterile cafeteria.
The latest dining options:
- Organic options
- Personalized menus
- Farm-to-table
- Wine pairing dinners
- Flexible dining times (not everyone wants to eat at 5 pm — especially Boomers)
- Tech to order room service
✶ What you can do:
Start by upgrading one meal weekly to a fine dining experience with table service and a special menu. Based on resident feedback, gradually expand to more meals and introduce elements like personalized menus and wine-pairing dinners.

3. Gardens — Gardens create engagement opportunities for long-term care residents. For some, gardens feel like home and are a cherished pastime.
Nursing homes with gardens let residents take up a hobby and share common interests, which promotes socialization.
Gardens also promote physical activity, which is life-altering for residents.
Gardening practices can be easily tweaked to cater to older people. You can install benches, incorporate raised beds, and have easy access to water.
A study of 470 nursing home residents who had access to an outdoor garden experienced:
✶ What you can do:
- Build a small garden area with raised beds and easy access. Start with a few easy-to-maintain plants and involve residents in planting and caring for the garden. Expand the garden based on interest and participation.

4. Physical Therapy — Based on the phrase, “use it or lose it.” Anyone who’s worked out for a while and then stopped can tell you this is 100% true.
Muscles require regular exercise to retain their strength. This is especially true for older people, who are at higher risk for falls and accidents because of a lack of exercise and mobility.
Wellness-centered long-term care facilities have on-site physical therapists to counteract muscle deterioration and prevent falls. These facilities also have gym equipment such as treadmills and dumbbells.
Many also offer exercise classes such as yoga and tai chi. These activities can be modified to accommodate less mobile individuals.
✶ What you can do:
- Introduce regular group exercise sessions, such as chair yoga or tai chi, accessible to all residents. Consider bringing in a physical therapist once a week for consultations and personalized exercise plans.

5. Occupational Therapy — Occupational therapists address not only the physical skills of residents but also the psychological and social aspects of their lives.
An occupational therapist’s primary goal is to improve residents’ quality of life so they feel more fulfilled, productive, and independent. They work with residents' limitations by teaching them new skills necessary to complete everyday tasks.
Occupational therapists are particularly beneficial for residents going through stroke recovery and those with dementia or Parkinson’s Disease.
Some residents need help learning to complete daily tasks with new medical equipment. Others may need help learning to manage their finances.
Occupational therapists fill these gaps and can connect residents with other resources like a social worker.
✶ What you can do:
- Start by offering workshops on daily living skills, such as using new medical equipment or managing finances. Based on resident needs, expand to individual occupational therapy sessions.

6. Arts & Entertainment — Some nursing homes offer residents music entertainment from their younger years. Musicians might play during dinner or a special event for residents to enjoy.
Residents with dementia or Alzheimer’s benefit from listening to music from their earlier years because their internal lives mainly consist of distant, long-term memories from their youth.
Updated art projects are also a new trend in long-term care. Creating art can help improve residents’ cognitive function and motor skills and help them cope with change and anxiety. Some facilities offer pottery classes, painting classes, and jewelry-making classes.
✶ What you can do:
Organize monthly music events featuring genres popular among residents. Begin an art program with simple projects like painting or jewelry making, and gradually introduce more complex activities.

7. Technology — Another nursing home trend is the inclusion of technology. Some nursing facilities now offer their residents free Wi-Fi.
Technology can help residents stay in touch with relatives, learn new skills, and keep up-to-date with cultural events. Some nursing homes also offer YouTube activity time where residents watch comedy skits or study genres of music.
Technology is also helpful for residents with dementia and Alzheimer’s. Many apps can help these residents create familiarity. Some apps allow you to create a virtual storybook of memories using film, music, and photos.
Other valuable tech used in skilled nursing facilities include wearable tracking necklaces and fall alarms. These devices let nurses on staff know where a resident is at all times. This is especially vital for residents with memory conditions that would cause them to wander and potentially get lost.
✶ What you can do:
- Provide residents with internet access to a communal tablet or computer. Start a weekly "tech hour" where residents can learn about using devices and apps and gradually introduce more technology-based activities
Nursing Home Staff Statistics
Let’s shout out to all the dedicated nursing home staff. Many nursing home employees find fulfillment in their roles, getting satisfaction from providing care and support to elderly residents.
While uber rewarding, this industry has challenges O’plenty. Overwork and burnout are significant concerns, made worse by staffing shortages and the demanding nature of the job.
- 94% of nursing homes face staffing shortages.

- Nursing homes have lost nearly 229,000 caregivers (more than 14% of their workforce) since February 2020.
- Culture Matters — Nursing homes’ annual staff turnover rates ranged from 65% to 100% before revamping their culture. After a culture upgrade, turnover rates dropped to 30%.
- The average nursing home reported a turnover rate of 53.3% among nursing staff and 51.9% among RNs.

- According to the American Health Care Association (AHCA), as of August 2021, there were over 80,000 vacancies for registered nurses and certified nursing assistants in nursing homes across the United States.
Nursing home staff who chose to stay at their jobs after the pandemic cite 2 reasons:
- Feeling appreciated for the job they do
- Receiving support from supervisors in the way of:
- Communication
- Scheduling
- Being able to go to them with a problem
✶ What you can do:
- Recognition Programs: Start with a simple recognition program, like "Employee of the Month" awards or thank-you notes from residents and their families. Gradually expand to more formal recognition events and rewards. Kudos go a long way with staff.
- Supportive Communication: Encourage open communication between staff and management. Start with regular check-ins or team meetings to discuss concerns and feedback. Gradually introduce more structured communication channels — possibly suggestion boxes or employee surveys.
- Flexible Scheduling: Begin by offering some flexibility in scheduling, such as allowing staff to swap shifts or request time off in advance. Slowly work towards more comprehensive scheduling solutions, like self-scheduling systems or offering part-time positions to accommodate personal needs.
- Staff Development: To get the ball rolling, offer occasional training sessions or workshops on relevant topics. Gradually expand to a more structured staff development program, including opportunities for professional growth and career advancement.
- Wellness Programs: Introduce simple wellness initiatives, such as regular breaks and access to healthy snacks. Then, build more comprehensive wellness programs, including mental health support, stress management workshops, and fitness activities.
FAQ
What percentage of Americans end up in a nursing home?
About 5 out of every 100 Americans may live in a nursing home.
Who is most likely to be in a nursing home?
Older people, especially women and those who need help with daily activities or have health problems are more likely to be in a nursing home.
Why do nursing homes have staffing shortages?
Nursing homes have staffing shortages because the jobs are demanding, there aren’t enough workers, and many caregivers leave their jobs due to feeling overworked and unsupported.
What age do most people go into a nursing home?
Most people go into a nursing home when they’re older, usually around 80 years old or more.
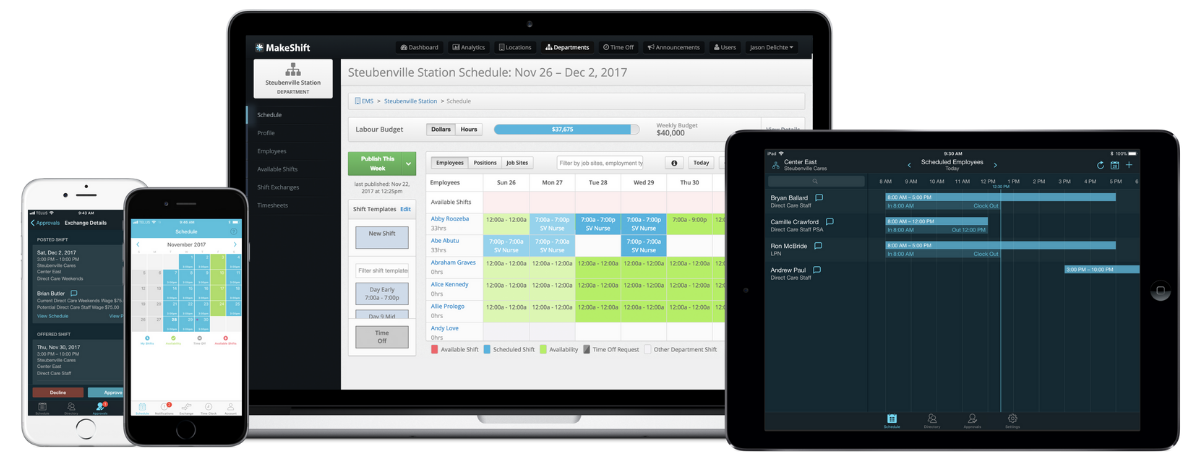
MakeShift Elevates Nursing Home Staff Scheduling
MakeShift takes a people-first approach to staff scheduling that goes beyond simple shift planning. Based on the nursing home staff statistics above, it’s obvious that you need to take extra measures to ensure your staff’s well-being is prioritized.
We offer smarter scheduling that creates an interactive conversation between you and your team. Your staff will appreciate having a say in their schedules, which will contribute to better work-life balance and higher retention.
1. View and manage schedules on the fly
Your staff can access their schedules, set availability, and submit requests on their phone. You can manage scheduling and approve requests on the go. Mobile accessibility makes scheduling more interactive and lifestyle-friendly.

2. Rotation-based scheduling
Easily create a rotating shift schedule to distribute the workload evenly. This helps squash staff burnout and fatigue and ensures that on-the-clock staff are mentally fresh. Rested and refreshed staff can offer more empathy when caring for your residents.

3. Compliance
There’s a lot going on in long-term care facilities, and it can be tough to stay compliant through manual monitoring. Ensure compliance with labor laws and regulations, including overtime rules and automatic fatigue alerts.
MakeShift is also HIPAA-compliant.

4. Improve staff communication
MakeShift provides a centralized platform for staff communication, which can help reduce scheduling conflicts and improve staff engagement.
With features like shift swapping and availability tracking, MakeShift empowers your nursing home staff to work together to fill staffing gaps and ensure everyone's needs are met.

5. Streamline scheduling processes
MakeShift Scheduling automates many of the time-consuming tasks associated with scheduling, such as shift creation, employee availability, time-off requests, and schedule distribution.
This saves time and reduces the administrative burden of scheduling.

Let the Stats and Trends Guide You
Running a quality nursing home can be overwhelming. Not to mention the constant evolution of long-term care, the aging population’s needs, and your staff’s well-being.
Rather than be overwhelmed by all the latest long-term care statistics and trends, let them guide you as you prep your facility for the future.
Choose areas that need the most attention and improve those first.
When you’re ready to upgrade your employee experience through innovative scheduling, we’re here to help. Schedule a FREE demo to see how MakeShift removes the overwhelming task of scheduling.